So value-based cancer care has arrived. Even with added resources and funding, early participants in value-based programs like the Oncology Care Model are already facing the complexity of reducing the cost of cancer care. With so many factors contributing to the cost of cancer treatment – many outside the control of the care team like drug prices, comorbidities, disease progression and more – it can be difficult to know where to start.
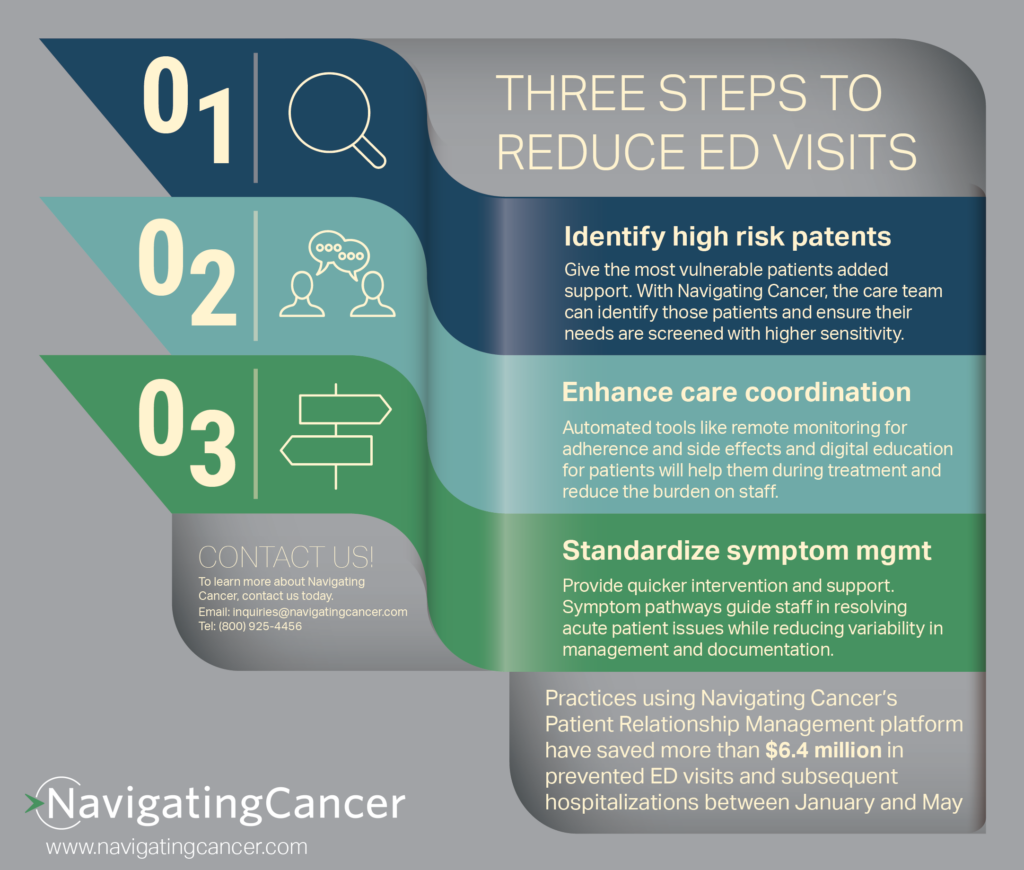
A promising opportunity for providers to reduce costs? Reducing unnecessary emergency department visits and subsequent hospitalizations. These often occur because high risk patients are treated the same as other patients, because a side effect worsens after hours or due to ineffective symptom management. A comprehensive Patient Relationship Management platform can give the care team to tools they need to keep patients out of the hospital, improve the patient experience and potentially improve outcomes.
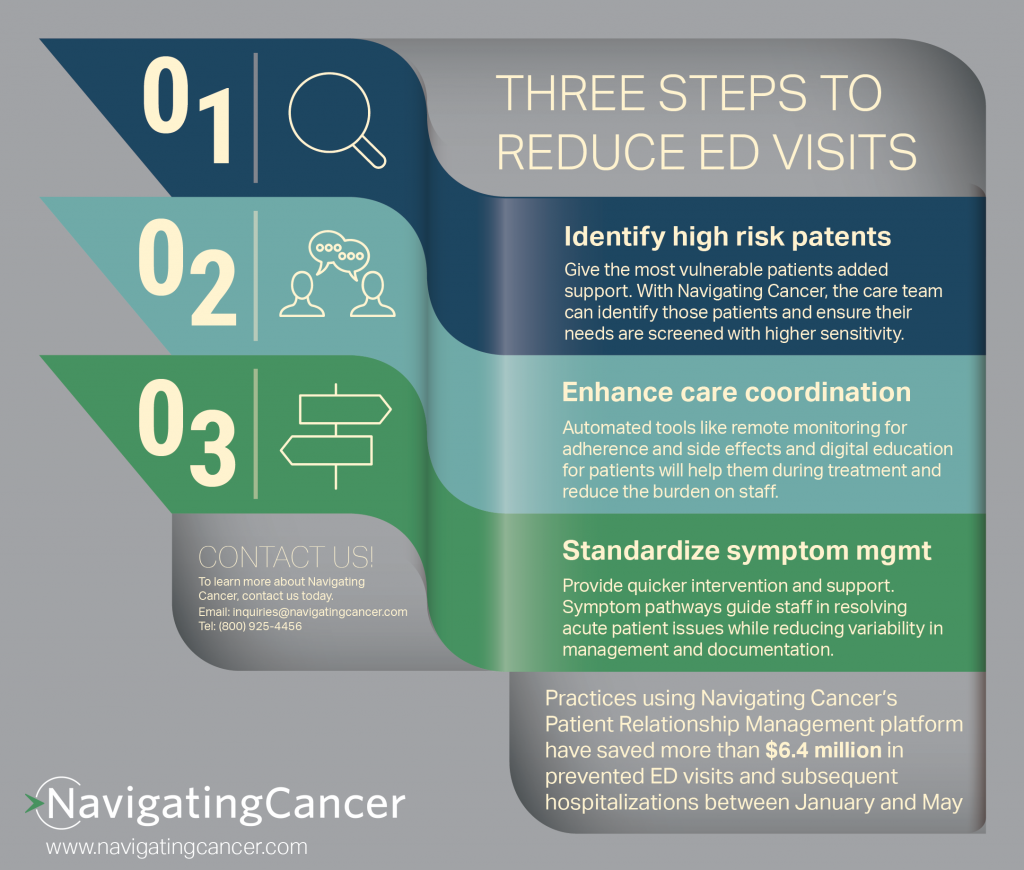
- Identify high risk patients. Different patients may require differing levels of attention and assistance during treatment. Identifying those patients at the outset is important, but can be tricky to keep track of in a busy practice. Leveraging a technology solution to flag patients as high risk ensures they don’t get overlooked. When a patient is designated as high risk in the Navigating Cancer platform, that patient’s needs are weighted more heavily and will be automatically prioritized with more sensitivity. A high risk patient reporting a “moderate” side effect registers as “severe” on the triage nurse’s workboard so they can provide quick intervention before the situation worsens.
- Enhance care coordination. Giving patients extra support during treatment will also contribute to a reduction in emergency department visits. That includes after hours support, psycho-social assistance and remote monitoring. Each of these gives the care team extra insight into what’s happening with the patient when they are not in the clinic and allows them to proactively intervene when needed, whether it’s worsening depression or an unmanaged side effect. Navigating Cancer’s platform makes all patient-reported outcomes visible to the entire care team as well as giving regular hours staff and after hours support the same view of the patient. This keeps everyone in the loop and, again, gives the care team extra insight to know when a patient is in need.
- Standardized symptom management. Cancer therapies can cause a wide variety of side effects and they each need to be managed in a consistent and comprehensive way. In addition, with new therapies and combinations, there is a lot to keep track of. With Navigating Cancer’s standardized pathways that are built right into the triage functionality, nurses don’t have to try to keep track of every best practice or remember every question they should ask the patient. They can use the integrated pathways to guide the conversation and ensure that they understand what’s happening with the patient, the severity of the situation and what action is called for.
Navigating Cancer’s Patient Relationship Management solution is an effective tool for care teams. It enables early intervention for patients and helps them avoid the emergency department – one practice reported preventing over 150 emergency department visits in three months.