
Principal Care Management (PCM)1 is designed to reimburse specialty practices for providing needed care management services to their patients. It enables oncology practices to continue providing the care coordination and planning necessary for quality patient care. PCM allows billing for provider and clinical staff time for essential care management functions, including medication management, referral coordination, and transitions of care. These services can be offered to the majority of your Medicare chronic care patient base.2
Oncology staff who provided necessary care planning and navigation activities can continue to provide those same services using the PCM billing codes. These services include (but are not limited to):
- Creation, maintenance, revision and monitoring of a disease-specific care plan.
- Managing care transitions and referrals.
- Medical and psychosocial needs assessments.
- Coordination of preventive services.
- Medication reconciliation, management and oversight of self-management.
- Creation and exchange of continuity of care documents.
- Coordination with home and community-based care.
- 24/7 On-call Services
These services are designed to occur outside of a patient visit. Practices are required to offer asynchronous communications, such as secure messaging, to provide PCM-related services. Clinic staff can use the current secure messaging Navigating Care platform to engage and communicate with PCM participating patients.
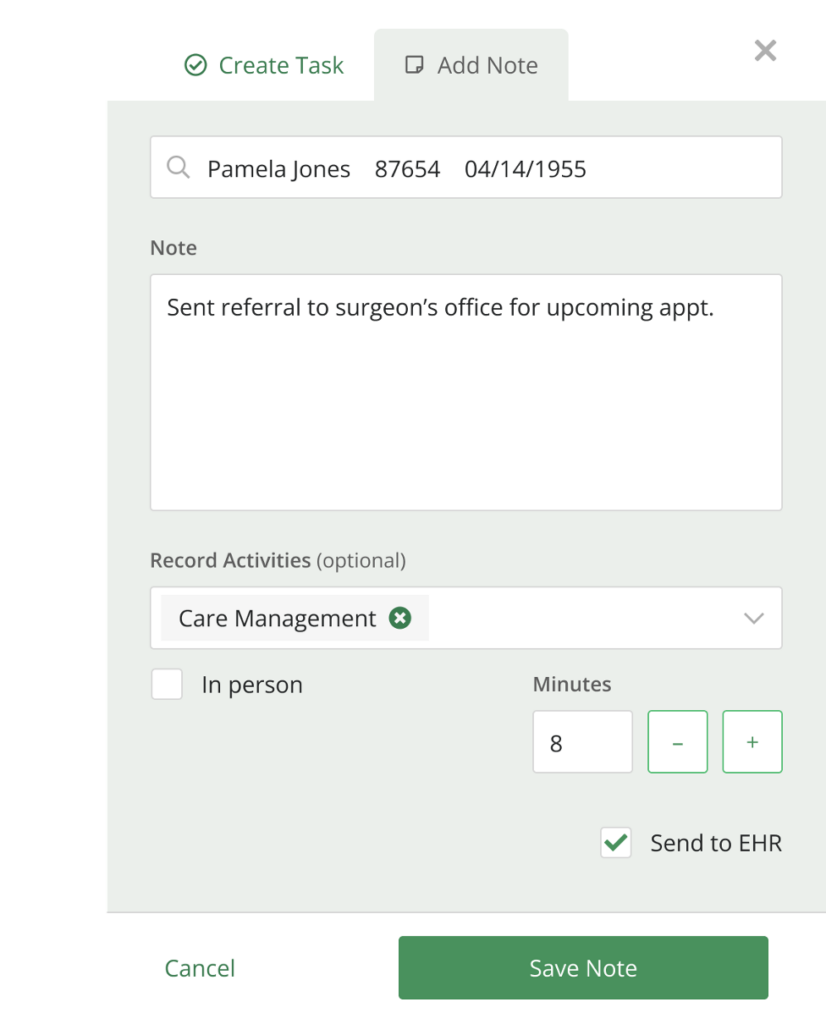
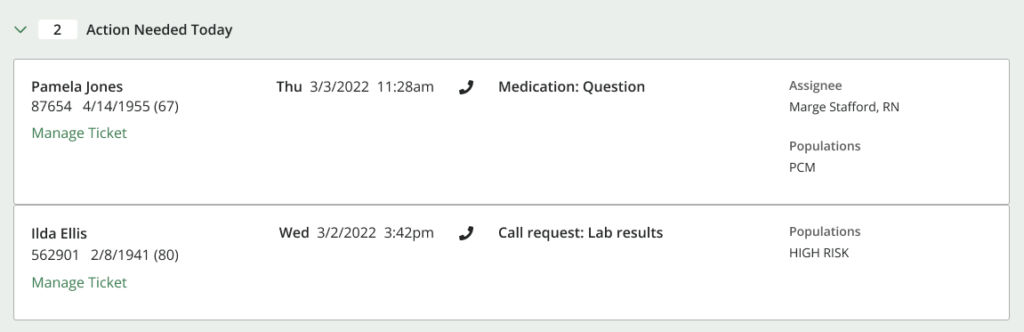
Our PCM/CCM product enhances and simplifies care management workflows for clinical staff. Clinical staff familiar with our platform can use those same tools to easily track time and activity notes within Navigating Care, as well as assign tasks to appropriate team members and incorporate those notes in the patient record. Practices can also readily identify which patients need follow-up services and efficiently organize their patients.
Providing PCM services to your patients offers an opportunity to enhance the quality of care and services to your patients between visits. Utilizing existing tools and workflows, and managing your PCM program through our Navigating Care PCM/CCM product can enable reimbursement for valuable clinical staff time.
The PCM beneficiary population encompasses a broad array of cancer patients, with few limitations on eligibility. Instituting a PCM program will work in tandem with private payor care management programs, and the services you provide through PCM are complementary to those required for eligible EOM beneficiaries, so you can have consistent workflows across your patient base.
Navigating Cancer has products and services to support oncology practices in providing quality care management to their patients. To learn more about instituting PCM at your practice, please contact us today.
1The CMS Chronic Care Management (CCM) Services MLN Booklet provides useful information, billing codes, and checklist for CCM and PCM.
2For more information on eligibility for Principal Care Management see our prior PCM blog article.platform