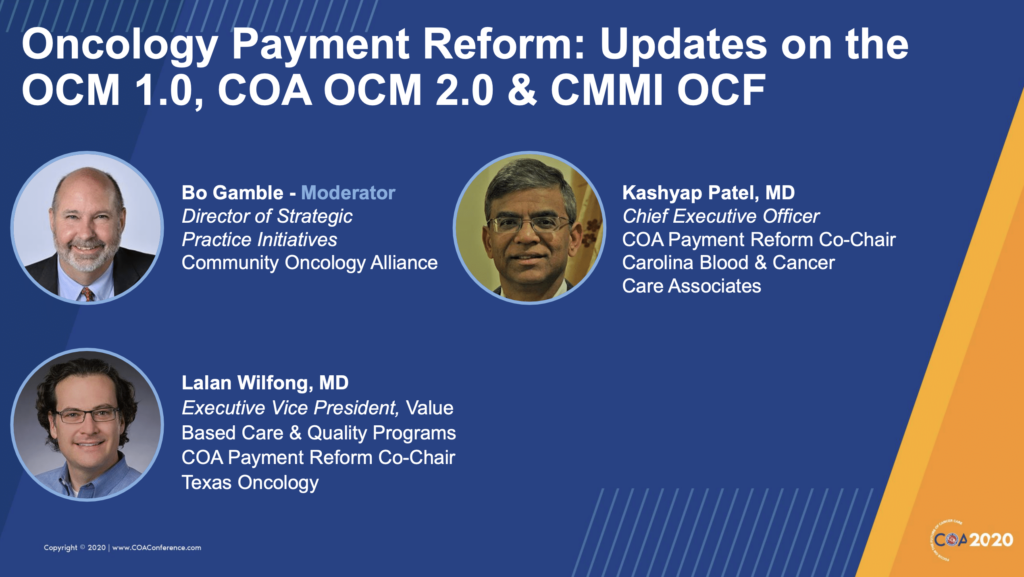
In a panel at Community Oncology Alliance’s (COA) recent virtual conference moderated by COA’s Director of Strategic Practice Initiatives, Bo Gamble, Kashyap Patel, MD, of Carolina Blood & Cancer Care Associates and Lalan Wilfong, MD of Texas Oncology recently shared an update on payment reform. These leaders in value-based cancer care are also the COA Payment Reform co-chairs so they brought some unique insight to this topic.
The shift to value-based cancer care has been a slow one, but a recent COA survey of 175 CMMI’s Oncology Care Model (OCM) participants, the 68 responses seemed to indicate growing acceptance of the fact that value-based programs are here to stay. Nearly 37% of the survey respondents reported that they moved into the two-sided risk arrangement in the model even though 32% had never received a performance payment. This suggests they expect to continue to improve their performance in the model and succeed in future performance periods.
“Once you trim the fat, there’s a point where there’s no more fat to trim. At some point you have think about rewarding those practices for doing the right thing.” ~ Lalan Wilfong, MD
The future of CMMI’s Oncology Care Model and Oncology Care First Model
Dr. Wilfong also pointed out that value-based care has never been more important. The COVID-19 crisis is resulting in growing unemployment and more patients needing healthcare through a government program – value over volume has to be the focus. However he also made the point that in these unprecedented times, 2-sided risk arrangements should be waived for the year to minimize administrative burdens and allow cancer care providers to focus on patient care.
He also emphasized that doing anything new right now would be very difficult, casting some doubt on the feasibility of CMMI’s proposed successor to OCM, the Oncology Care First Mode (OCF). To ensure cancer care providers are able to get through the current crisis and also remain whole, he encourages a focus on savings and less on gainsharing for the time being. For providers who have done well in value-based care models like OCM, Dr. Wilfong pointed out that there isn’t a lot of waste to trim and providers should be rewarded for doing the right thing.
What about other proposed alternative payment models?
COA is working to help shape these models and provide input on behalf of its membership. While its proposed model OCM 2.0 has not been adopted, they are still advocating value models – to both CMS and private payers – to include 3 tiers that take into account a practice’s experience and aptitude for complexity: entry, intermediate, and advanced. This would enable more participation and move cancer care as a whole toward common goals like reduced ER visits, higher quality care, and lower cost of care.
The presentation included a table of what they would like CMMI to consider for the OCF and it highlights some concerns that likely many providers have: transparency about payments, mandatory 2-side risk for OCM participants, drug prices, adjustments for novel therapies, and the uncertainty around how the Monthly Prospective Payment, which would be a significant change for practices.