Navigating Cancer’s President and Founder, Gena Cook, spoke at the recent ACCC Annual Meeting and Cancer Center Business Summit on the topic of electronic patient-reported outcomes in the context of value-based care. The value of the patient voice in cancer care as well as the importance of technology to keep patients and care teams connected were both key themes during the conference and Gena’s talk added some important context.
It’s widely acknowledged that the United States healthcare system is unsustainable, yet the innovations in cancer are significant. In the context of value-based care, innovators have demonstrated that they can help patients have better outcomes while ensuring we reduce waste and inefficiency with better patient management with enhanced services. However, while many pilots were able to reduce costs, including ED visits and hospitalizations, they did so only with small patient populations and manual processes and it’s just not sustainable to rely on extra people, sticky notes, excel spreadsheets, and outlook calendar reminders to meet value-based initiatives.
Improving cancer care with technology
Gena shared how Navigating Cancer has been working for over a decade to build technology that can support the people and processes that have been shown to be impactful – but do so in a sustainable way. She shared that there is now evidence, including an ASCO abstract and a study published in the Journal of Oncology Practice that quantifies the impact of the Navigating Cancer solution. Navigating Cancer’s digital platform is helping improve outcomes and help patients avoid the utilization of emergency services and hospitals. In addition to building evidence, Navigating Cancer’s customers are also an important source to better understand what can be automated, what would make clinical workflows more efficient and how we can help strengthen the connection between patients and their care team.
When patients know what to do, and when to call their doctor, it does result in a reduction in cost. Over the last 10 years as the healthcare system has tried to move towards value-based care, the first step was practice transformation – taking care of patients in a new, personalized way. Then we were able to work on technology transformation. Now we’re trying to figure out how we can truly involve the patients in the shift to value-based care.
So why are patient-reported outcomes important for value-based care?
Gena next highlighted what the research has shown and what we’ve seen implementing a ePRO program for our customers. Leading researcher and scientific advisor to Navigating Cancer, Ethan Basch, MD, MSc has been studying ePROs and cancer care for 10 years and he’s consistently found monitoring patients between visits has a significant impact on reduction of ED visits and hospitalizations, survival, adherence, and patient satisfaction.
Gena then asked the audience to consider the power of an ePRO tool can be as powerful as many new drugs. It was reported in JAMA that from 2002 to 2014 new therapies had 2.1 months overall survival impact and the clinical trial of Yervoy showed a survival benefit of four months. Adding an ePROs program could make those new therapies more effective and successful.
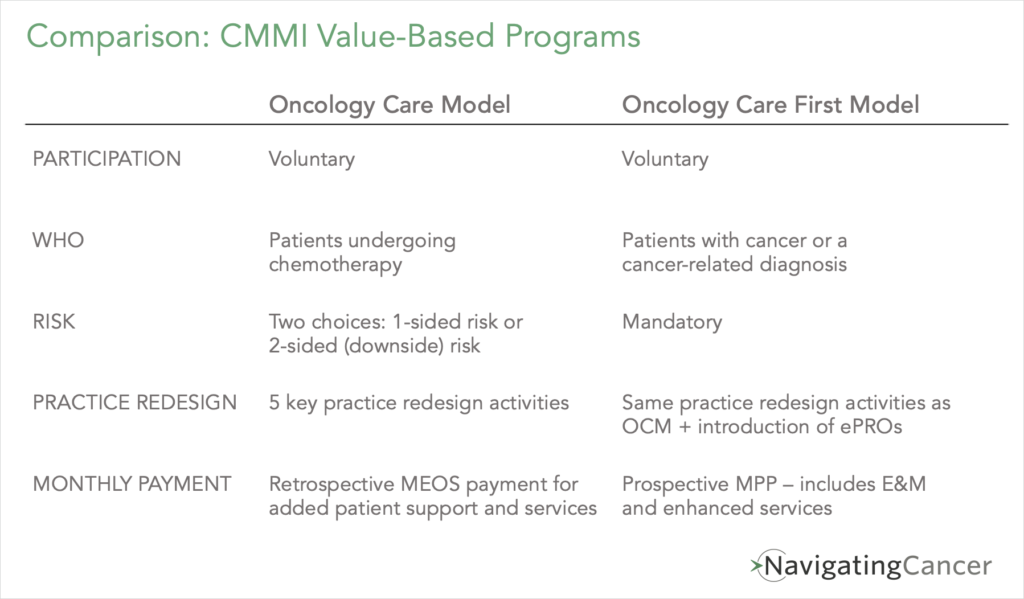
Taking on Risk in Value-Based Care
Community Oncology Alliance recently published the results of a survey they conducted with participants in the Oncology Care Model as practices were deciding about their participation in the program. For OCM practices moving to two-sided risk – 32% of practices who are moving to two-sided risk have not yet received a performance payment in the program. But instead of leaving the program they are essentially becoming payers by taking on downside risk. So it seems apparent that many see that the future is value-based care and the stakes are high. Providers will need technologies like Navigating Cancer’s to succeed. And OCM’s successor the Oncology Care First Model (OCF) will similarly require high quality, comprehensive care and will likely add ePROs to make that connection to the care team even more streamlined:
In looking to the future in light of the changes in cancer care, Gena shared a bit more about integrating PROs into value-based care. There are a lot of perceived barriers about implementing ePROs in clinical practice:
- Will patients participate?
- How do I incorporate this into the workflow?
- Who is going to manage the process?
But the research shows that patients are hesitant to report their symptoms and as providers take on more risk, knowing what’s happening with patients when they are away from the clinic is essential for proactive care and helping patients avoid unnecessary ED visits and hospitalizations.
Integrating ePROs into the clinic workflow
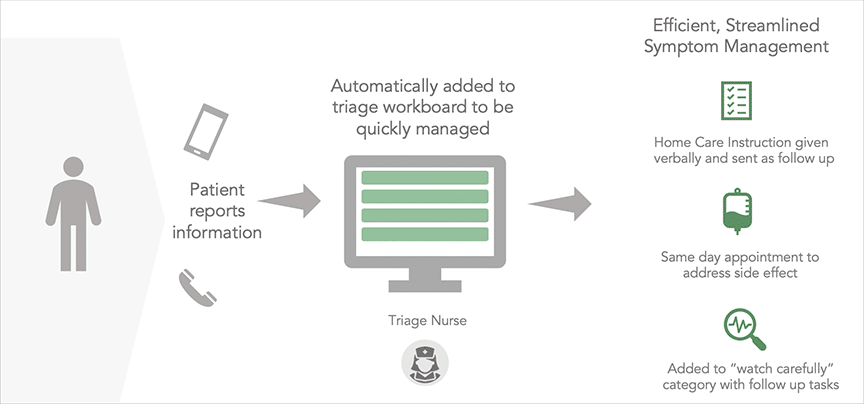
When it comes to integrating an ePRO program into clinical practice, Gena referred to the Advisory Board’s recommended best practice for triage, which includes a dedicated triage nurse who is able to help patients in real time using standardized triage pathways using a tool like Navigating Cancer. When a practice has that infrastructure in place, remote monitoring to collect ePROs is already integrated and monitoring and responding to PROs melds right into an existing workflow. Now you can deliver proactive care, manage high risk patients, and keep patients out of the hospital. Gena did highlight the importance of integrated, flexible workflows otherwise you could struggle to efficiently manage incoming patient issues.
Some Navigating Cancer customers who have implemented Health Tracker have reported a 50% reduction in inbound clinical call volume because they can reach the care team, are receiving assistance without calling back or are able to report via the ePRO program. Navigating Cancer has also typically seen as 18% reduction in ED visits. The old model of clinical nurses checking voice mails between patient visits can result in a 4 or 5 hour delay which often leads to an urgent care visit.
Gena concluded her remarks with some final thoughts. Technology is not a stand alone solution. Navigating Cancer is still developing tools to meet patients where they are – smartphone or not, patients can still be participants in their care. The technology just puts everyone, including the patient, on the same page.
Interested in learning more about Navigating Cancer? Contact us today.