Obviously in the current COVID-19 crisis, telehealth is getting a lot of attention. In the past week or so AJMC hosted “How COVID-19 Will Affect telehealth and Alternative Payment Models,” ACCC hosted “Telehealth Billing & Coding,” and COA hosted “Telehealth Expansion & Oncology Care: What You Need to Know.”
It’s clearly a hot topic – and for good reason. Cancer patients are particularly vulnerable to COVID-19. Keeping them away from the clinic – or worse, the emergency department – has become a primary goal for providers and telehealth presents a really great opportunity to achieve that. So why has it taken a pandemic for cancer care providers to widely adopt telehealth? Reimbursement, resistance to change, and lack of necessity were all cited as barriers before COVID-19.
To respond to the crisis, providers and CMS have acted quickly. CMS released its COVID-19 Regulatory Changes Interim Final Rule on March 30, 2020 (retroactive to March 1 – read about the key provisions) to address the current public health emergency (PHE) and healthcare providers were grateful. The speakers in one webinar thanked CMS, saying “telehealth has been a life saver” and “you have saved lives.”
Some of the changes in the interim rule include:
- Allowing providers to bill at the same rate for virtual visits as they do in the clinic
- Revising the definition of a telephone so that digital devices like iPhones can be used since they have video capability
- Extending coverage to telephone visits that were previously not coveredEnabling the physicians to provide virtual supervision where appropriate
- Waiving the visit co-pays during the crisis
These changes have enabled providers to move a very high percentage of their appointments to a telehealth format. Practices from all over the country reported launching their telehealth programs quickly – in some cases in a day or two. They also reported that patients were adapting well to the new technology and providers were also responding positively. While most of the speakers expressed things like “telehealth is here to stay” it is important to note that CMS’ rule would revert back at the end of the PHE.
The encouraging thing is these practices are looking at telehealth as a permanent tool for healthcare delivery now that this crisis has caused them to give it a try. Cancer patients, in particular, have a lot of appointments. If they live far from their clinic, are low income, can not take time off work – telehealth is an excellent option for visits that don’t need to be done in person. Keeping immunocompromised patients safe at home is another good reason. There are also fewer oncologists – this could enable them to see more patients.
So how is all of this impacting alternative payment models?
As one speaker pointed out, to date value-based payment models have been about receiving a bonus, rather than taking on risk and while fee-for-service is still around, telehealth may have a hard time persisting. This crisis was described by one speaker as an accelerant for value – we have to figure out how to reduce costs and enable financial success, rewarding providers for the best care. That could be the key for telehealth finally becoming the norm.
Remote monitoring is the next step for patient care
Electronic patient-reported outcomes (ePRO) are proven to reduce unnecessary emergency department visits and that’s never been more important than today.
And payers are signaling that ePROs are important to them too. The successor to CMS’ Oncology Care Model, the Oncology Care First Model, is slated to begin next year. While the current crisis will likely delay that, they intend to include ePRO as an additional practice improvement activity in the next model.
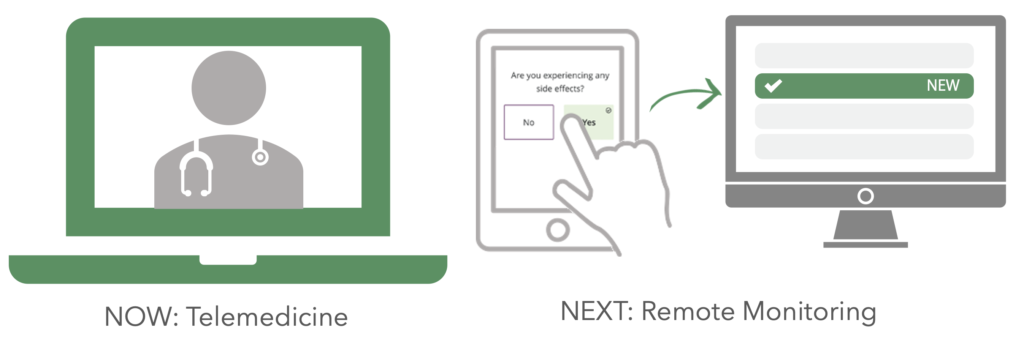
At Navigating Cancer, we see collecting ePROs as an extension of telehealth. The combination of in-person visits, virtual visits, and patient-reported outcomes give the care team the tools they need to keep patients safe, on therapy, and out of the hospital. We believe in meeting patients where they are. Expanding the methods patients have to reach their care teams is a good step forward for cancer care.
Interested in remote monitoring? Learn more about Health Tracker.
